Diagnostic Approach to Shoulder Pain
Shoulder pain is a common presenting concern in primary care. This is a big topic - but we will tackle some big take home points today that you can incorporate into your daily practice.
Case: you’re seeing a 47-year-old female with daily right shoulder pain for the last three months. She tells you it started to hurt after lifting a heavy box onto a high shelf at work. She frequently performs overhead activities with her job. She denies any recent falls or motor vehicle accidents. There is no history of shoulder injury or surgery. Past medical history is significant for diabetes, hypertension, and dyslipidemia. It is affecting her activities of daily living and work life.
Diagnostic Approach: approach to shoulder pain in primary care can be tricky. The shoulder joint is complex and the differential diagnosis is broad. We can narrow down our differential into three major buckets: traumatic shoulder injury, non-traumatic intrinsic shoulder pain, and non-traumatic extrinsic shoulder pain (1). From there, we can determine whether diagnostic imaging is warranted.
For all shoulder presentations, consider the following for history and physical exam.
BOTTOM LINE:
1. Determine if it is traumatic shoulder pain or non-traumatic shoulder pain.
2. If non-traumatic, is it intrinsic (coming from the shoulder, well localized pain) or extrinsic (not coming from the shoulder, poorly localized pain)?
History: age, history of trauma, history of previous shoulder injury, repetitive shoulder motion (e.g. with work, home, sports), pain history (location, quality, radiation, severity, timing, triggers), neck pain, neurologic symptoms (e.g. paresthesia, weakness) of the affected extremity, past medical history, and medications (2). If shoulder pain is well localized, the differential is narrowed down to intrinsic causes (1). If poorly localized, consider extrinsic causes of shoulder pain.
Physical exam: For MSK presentations, remember the basics - inspection, palpation, range of motion (active and passive), and special tests. Assess the joint above (neck) and joints below (elbow, wrist, hand), and perform a basic neurovascular assessment. Check out Rheum Tutor to refresh your examination skills.
Now let’s review our differentials for traumatic, intrinsic, and extrinsic shoulder pain.
1. Traumatic Shoulder Pain
Ask the following to help narrow down your differential:
BOTTOM LINE: For traumatic shoulder pain, rule out clavicle fracture, proximal humerus fracture, glenohumeral dislocation, and AC separation.
Did the patient fall directly onto the shoulder?
Was there blunt trauma to the shoulder? (e.g. collision sport, motor vehicle accident)
Did the patient fall onto an outstretched arm?
Do they have risk factors for adhesive capsulitis post-trauma? (e.g. diabetes)
Do they have risk factors for fragility fracture? (e.g. osteoporosis)
Differential Diagnosis for Traumatic Shoulder Pain
2. Non-Traumatic Intrinsic Shoulder Pain
I like to use the anatomic framework to work through my differentials. It is important have a basic understanding of shoulder joint anatomy. This is most likely what our patient is presenting with.
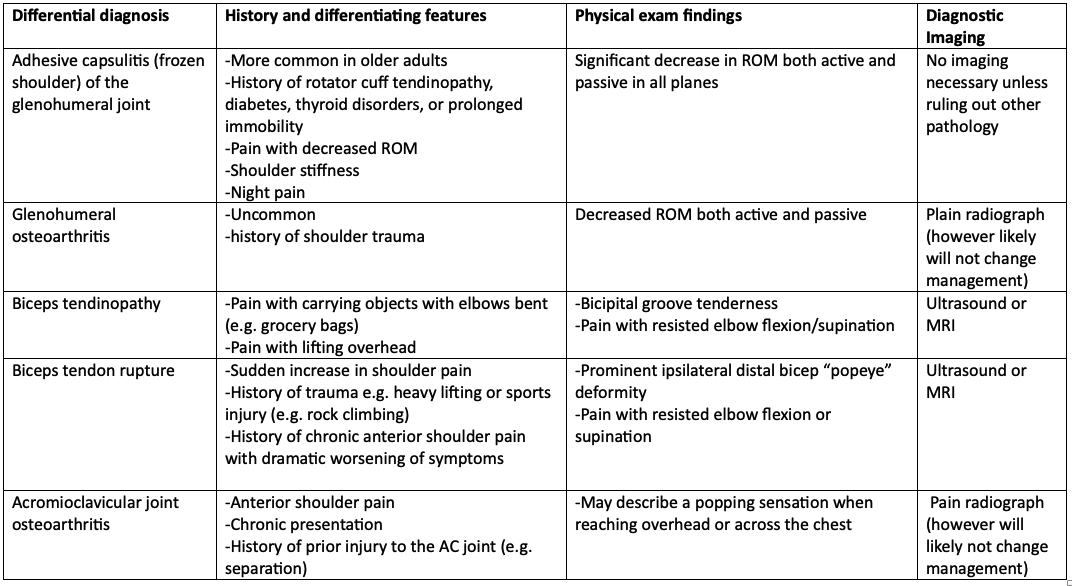
Differential Diagnosis for Non-Traumatic Intrinsic Shoulder Pain
Souces: Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part I. Evaluation and diagnosis. Am Fam Physician. 2008 Feb 15;77(4):453-60. PMID: 18326164. Vaughan A, Hulkower S. Evaluation of the adult with shoulder complaints. In: UpToDate, Eidt Fields K, Grayzel J (Ed), Wolters Kluwer. (Accessed April 10, 2024).
BOTTOM LINE - For non-traumatic intrinsic shoulder pain, think GARB:
Glenohumeral joint: frozen shoulder and glenohumeral osteoarthritis
AC joint: osteoarthritis, strain or separation
Rotator cuff: tendinopathy, tear, or shoulder impingement (most common)
Biceps tendon: tendinopathy or tear
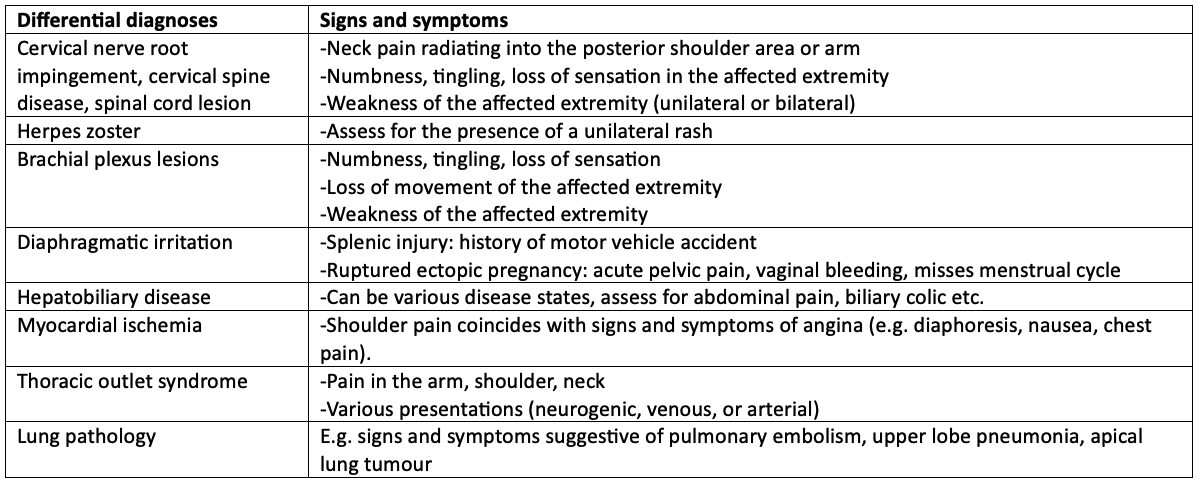
3. Non-Traumatic Extrinsic Shoulder Pain
There a long list of differential diagnoses. Extrinsic pain is often poorly localized. If the pain is vague, rule out a thoracic or abdominal source, if the pain is sharp with radiation consider a neurological source (1).
Differential Diagnosis for Non-Traumatic Intrinsic Shoulder Pain
Back to the case: the pain is localized to the anterior shoulder, with subacromial tenderness on palpation. There is no bruising, swelling, or erythema. There is normal passive ROM in all planes, and pain is reported with resisted external rotation and abduction. There is no weakness on strength testing. You elicit a positive hawkin’s test, apley scratch test, and negative drop arm test. You palpate brachial and radial pulses, and sensation is grossly intact. The remainder of the physical exam is unremarkable. You suspect rotator cuff tendinopathy and possibly shoulder impingement, and question whether diagnostic imaging is warranted.
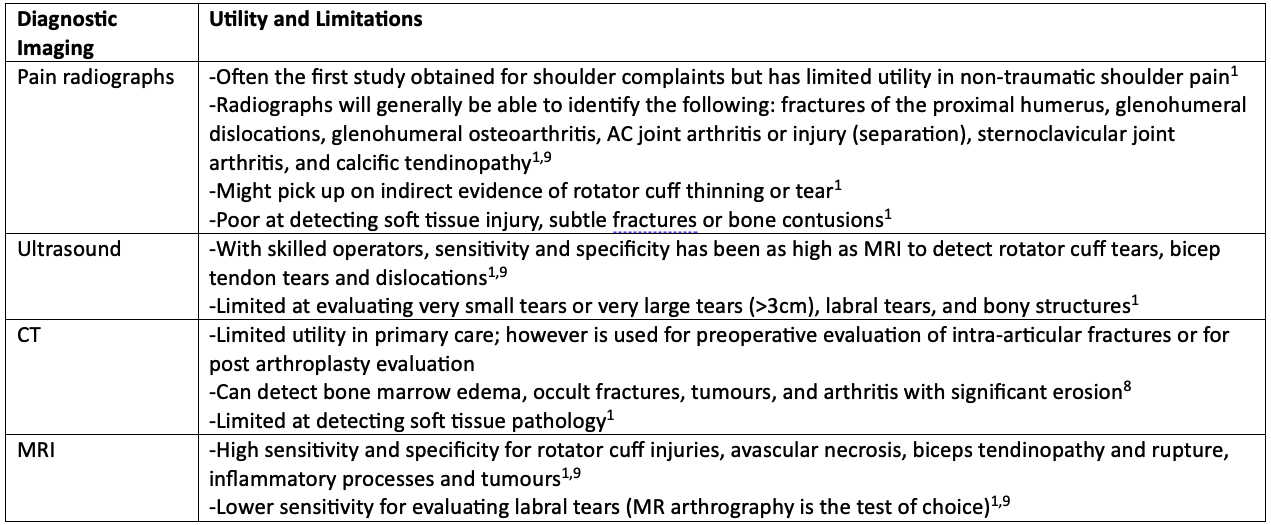
Role for Imaging: A General Overview
Back to the case: Since the shoulder pain has been present daily for 3 months and is affecting her activities of daily living and work life, you decide to send her for a shoulder ultrasound to confirm your suspicion for rotator cuff tendinopathy (and rule out partial tears and assess the extent of damage). In the meantime, recommending intensive physiotherapy is paramount to aid in rehabilitation.
BOTTOM LINE:
X-ray: good for fractures and dislocations, but will miss soft tissue injuries, subtle fractures and bone contusions.
Ultrasound: a good place to start for rotator cuff and biceps tendon pathology. It may miss small tears. Go to MRI if imaging is negative and your index of suspicion remains high.
MR: gold standard test for rotator cuff pathology and other soft tissue injuries.
MR arthrography: gold standard test for labral tears.
That was a hefty topic! Good on you if you read through the entire post.
Key take home point: isolate where you think the shoulder pain is coming from, determine whether it’s traumatic or non-traumatic, and ask whether diagnostic imaging will change your management (e.g. are they a surgical candidate or is conservative management for 6-8 weeks reasonable?)
References/readings:
Up to date: Vaughan A, Hulkower S. Evaluation of the adult with shoulder complaints. In: UpToDate, Eidt Fields K, Grayzel J (Ed), Wolters Kluwer. (Accessed April 10, 2024).
Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005 Nov 12;331(7525):1124-8. doi: 10.1136/bmj.331.7525.1124. PMID: 16282408; PMCID: PMC1283277.
Clavicle: Bentley TP, Hosseinzadeh S. Clavicle Fractures. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507892/
Proximal humerus: Pencle F, Varacallo M. Proximal Humerus Fracture. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470346/
Glenohumeral dislocation: Abrams R, Akbarnia H. Shoulder Dislocations Overview. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459125/
AC separation/strain: Kiel J, Taqi M, Kaiser K. Acromioclavicular Joint Injury. [Updated 2022 Sep 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493188/
Sternoclavulcular subluxation/dislocation: Kiel J, Ponnarasu S, Kaiser K. Sternoclavicular Joint Injury. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507894/
Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part I. Evaluation and diagnosis. Am Fam Physician. 2008 Feb 15;77(4):453-60. PMID: 18326164.
Canadian Association of Radiologists. Canada. 2021-2022 [April 2024]. Available from https://car.ca/patient-care/referral-guidelines/