When to Order Imaging for Male Patients with Lower Urinary Tract Symptoms
Case: You are seeing a 70-year-old male with a 6-month history of lower urinary tract symptoms (LUTS) including urinary urgency, frequency, straining, and feeling of incomplete emptying.
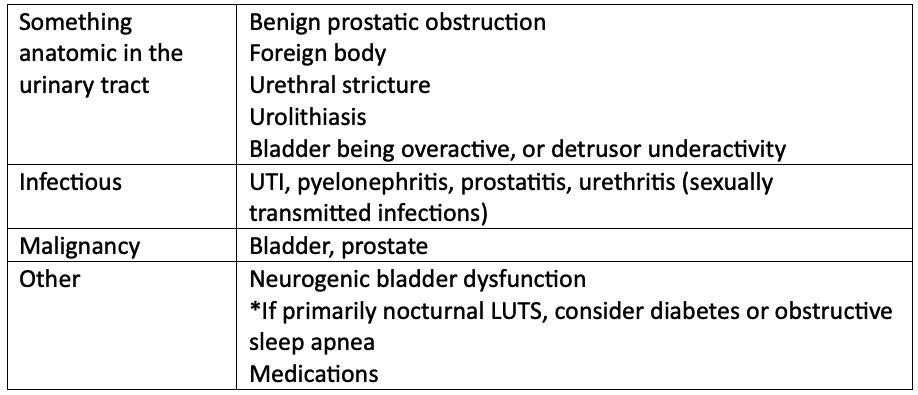
What is LUTS? It is a general term that encompasses several different symptoms (e.g. urgency, frequency, straining, and the feeling of incomplete emptying). There are many different causes of LUTS.
Back to the case: upon further questioning, he says he has developed intermittent low-grade fevers, malaise, and myalgias within the last week, which prompted his visit today. He did void about 1 hour ago. He has no history of surgery and does not take any medications. His vitals are stable, his abdomen is soft and non-tender, there is no CVA tenderness, however you palpate an enlarged prostate on exam without nodules or bogginess. He finds the exam uncomfortable but not exquisitely painful.
Diagnostic Approach: what other differential diagnoses should we consider in this case? (1)
Red flags: unable to void (acute urinary obstruction), systemically unwell (e.g. high fevers, nausea, vomiting etc.), LUTS with severe back pain (cauda equina, spinal metastasis)
Back to the case: based on his age, sex, history, and physical exam, your main differential is UTI. You know UTIs are not common in males unless there is an underlying cause – like benign prostatic obstruction.
Initial testing: You start with a POCT urine that reveals hematuria, proteinuria, leukocytes, and nitrites, confirming your suspicion for UTI. You start treatment, but is any other testing needed at this time?
Initial work up for LUTS: According to the Canadian Urological Association and the American Urological Association, if a male presents to you with LUTS, start by obtaining a comprehensive medical history, physical exam including DRE, and administer the International Prostate Symptoms Score (IPSS) (2, 3). The severity of symptoms (mild, moderate, or severe) will guide your treatment recommendations (2). A urinalysis helps rule out other diagnoses other than benign prostatic enlargement (2). PSA testing should be offered to patients who have at least a 10-year life expectancy, and for whom the knowledge of prostate cancer would change management (2). Take caution in ordering a PSA right away if a patient is presenting with UTI, prostatitis, or recent prostate stimulation (e.g. vigorous exercise like cycling) – as PSA can be falsely elevated.
Back to the case: you hold off on ordering PSA testing until the infection has cleared. What about diagnostic imaging?
Role for Imaging in LUTS: ordering post void residual (PVR) and/or uroflowmetry is warranted in this case, as you are concerned with outflow obstruction. It is also reasonable to order if there is any diagnostic uncertainty. The preferred method to assess PVR is with a pelvic ultrasound or a specific bladder scan unit (4).
These tests help determine the bladder’s baseline ability to empty, can identify severe urinary retention requiring urgent medical therapy, and can reveal detrusor dysfunction (3). There is no universally accepted definition of clinically significant PVR, however a persistent PVR of >100ml or increasing PVR over time may predict acute urinary retention or poor response to medical treatment (3, 4).
KUB ultrasound is not routinely ordered in males with LUTS, however, if there is any suspicion for urolithiasis, history of UTI, hematuria, or other complicating history, this should be considered for further evaluation (4).
What about CT abdomen and pelvis? There is little relevant literature on the role for CT in the initial evaluation of LUTS (4), unless you are wanting to rule out urolithiasis.
What about MRI? There is little relevant literature on the role for CT in the initial evaluation of LUTS, but has a role in evaluation for prostate cancer (best left for our urology colleagues!) (4).
Back to the case: you start with a pelvic ultrasound, PRV, and KUB ultrasound given the UTI and hematuria. PVR is elevated at 200mls, but there is no hydronephrosis or other structural abnormalities on KUB ultrasound. This likely confirms benign prostatic obstruction. In follow up, you repeat urinalysis and urine C&S to confirm eradication of organisms and discuss ordering PSA testing in 6-8 weeks. You revisit his IPSS score once symptoms have settled and discuss treatment options. (Subscribe to read this week’s newsletter which will review approach to PSA testing and treating LUTS!)
Key Take Home Points:
Start with the history, physical exam (including DRE), urinalysis and IPSS for any male that presents with LUTS.
Consider PSA testing using shared decision-making.
In cases where diagnostic uncertainty exists, or if a patient presents with a UTI, consider starting with a PVR and/or uroflowmetry.
References/readings:
Abdelmoteleb H, Jefferies ER, Drake MJ. Assessment and management of male lower urinary tract symptoms (LUTS). International journal of surgery (London, England). 2016;25:164-71. https://www.sciencedirect.com/science/article/pii/S1743919115013618
Elterman D, Aube-Peterkin M, Evans H, Elmansy H, Meskawi M, Zorn KC, et al. UPDATE--Canadian Urological Association guideline: Male lower urinary tract symptoms/benign prostatic hyperplasia. Canadian Urological Association journal. 2022;16(8):245-56.
American College of Radiology [Internet]. ACR Appropriateness Criteria Lower Urinary Tract Symptoms-Suspicion of Benign Prostatic Hyperplasia [2019]. Available from https://acsearch.acr.org/docs/69368/Narrative/