When to Order CT Sinus Imaging for Rhinosinusitis
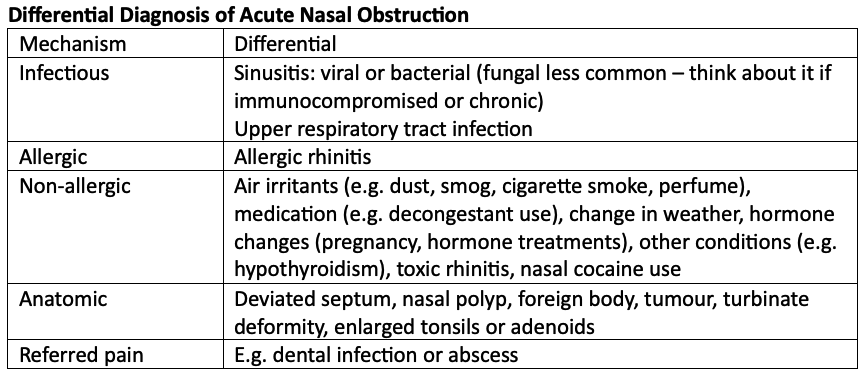
Case: Case: you’re seeing a 24-year-old male with a 14-day history of nasal obstruction. Before gathering more information, what is your differential diagnosis for acute nasal obstruction? I like to use the mechanism framework to organize my differential (1, 2).
Back to the case: He complains of pressure in his head and says symptoms have worsened in the last 3 days. He has tried intranasal steroids and a nasal saline rinse daily for the last week with minimal improvement. He has a fever of 40C (104F). He denies any nasal trauma, cough, shortness of breath, sore throat, or eye pain. He had a cold 2 weeks ago. He is alert and oriented, there is pain on percussion of his forehead, and nasal passages reveal thick purulent discharge. The remainder of your head, neck, and neurological exam is reassuring. He has a past medical history of allergic rhinitis and occasionally takes antihistamines. He denies a history of sinus infection. What is our most likely diagnosis?
Acute rhinosinusitis: <4 weeks.
Subacute rhinosinusitis: a continuum of acute rhinosinusitis >4 weeks and <12 weeks.
Recurrent acute rhinosinusitis: >4 episodes of an acute presentation, lasting at least 7 days each in any 1-year period.
Chronic rhinosinusitis: >12 weeks. (2)
Acute rhinosinusitis! What is it? it is an infection causing inflammation in the nasal mucosa and sinuses lasting less than 4 weeks (2). This leads to constriction of nasal passages, poor drainage of mucus, poor tissue oxygenation, and predisposition to microbial growth (3). Predisposing conditions include a recent viral upper respiratory tract infection, allergic rhinitis, nonallergic rhinitis, and rhinitis medicamentosa (3). Other medical conditions that are associated with acute rhinosinusitis may include pregnancy, hypothyroidism, cystic fibrosis, migraine, vascular headache and immunodeficiency (3). The following anatomic causes may predispose to development of acute rhinosinusitis: deviated septum, nasal polyps, nasal foreign body, tumour, turbinate deformity, enlarged tonsils or adenoids (3).
It is important to differentiate between acute, subacute, recurrent acute, and chronic rhinosinusitis, as management differs.
Diagnostic Approach: acute rhinosinusitis is a clinical diagnosis. Symptoms that are most sensitive and specific include purulent nasal drainage with either nasal obstruction or facial pain, pressure, or fullness (1). Isolated headache is not a symptom of sinusitis (with the rare exception of sphenoid sinusitis which can present as an occipital or vertex headache), but facial pressure is (1).
BOTTOM LINE: THINK “PODS” (PAIN/PRESSURE - OBSTRUCTION - DISCHARGE - SMELL CHANGES) TO DIAGNOSE ABS.
How do we differentiate between viral and bacterial rhinosinusitis (ABS)? Viral etiology is more common than bacterial rhinosinusitis (3). If symptoms persist beyond 7 days (3) (some guidelines propose 10 days) or if they worsen after an initial period of improvement (1), it is more likely to be bacterial. For a diagnosis of acute bacterial rhinosinusitis, the patient must have nasal obstruction, nasal purulence, OR discoloured post nasal discharge PLUS at least 1 of the following: facial pain, pressure, or fullness, hyposmia or anosmia (3). The “PODS” mnemonic can help you remember this (Pain/pressure, nasal Obstruction, nasal Discharge, Smell changes). Other symptoms may include fever, fatigue, headache, halitosis, malaise, dental pain, cough, and otalgia (2, 1).
BOTTOM LINE: ACUTE RHINOSINUSITIS IS A CLINICAL DIAGNOSIS. CONSIDER IMAGING IF THERE IS DIAGNOSTIC UNCERTAINTY, IF RED FLAGS EXIST, OR IF YOU SUSPECT RECURRENT ACUTE RHINOSINUSITIS OR CHRONIC RHINOSINUSITIS.
Role for Imaging: if a diagnosis of uncomplicated acute rhinosinusitis has been made without red flags, ordering imaging will not change management (3). Diagnostic imaging is helpful if red flags are present, if diagnostic uncertainty exists, or in the case of recurrent acute sinusitis or chronic rhinosinusitis.
When to refer? If red flags are present, in the case of recurrent acute sinusitis, or chronic rhinosinusitis that is failing medical management (5).
Back to the case: you rule out red flags and diagnose your patient with acute bacterial sinusitis clinically. No imaging is warranted at this time. You review treatment recommendations and give him return precautions.
Key Take Home Points:
Order imaging of the sinuses (preferably CT) if there is diagnostic uncertainty, in cases of recurrent rhinosinusitis or chronic rhinosinusitis (to assess for underlying anatomic abnormalities).
Refer to an urgent care setting if red flags are present (or consult ENT if you work in an urgent care setting).
How do we treat acute bacterial rhinosinusitis - antibiotics or no antibiotics?
Read more in this week’s newsletter – released Sundays!
References/readings:
DeBoer DL, Kwon E. Acute Sinusitis. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 31613481.
Battisti AS, Modi P, Pangia J. Sinusitis. 2023 Mar 2. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 29262090.
Kaplan A. Canadian guidelines for acute bacterial rhinosinusitis: clinical summary. Can Fam Physician. 2014 Mar;60(3):227-34. PMID: 24627376; PMCID: PMC3952756.
Canadian Association of Radiologists. Canada. 2021-2022 [2022; February 12, 2024]. Available from: https://car.ca/wp-content/uploads/Head-and-neck.pdf
Okuyemi KS, Tsue TT. Radiologic imaging in the management of sinusitis. Am Fam Physician. 2002 Nov 15;66(10):1882-6. PMID: 12469962.
Radiopedia. Chronic sinusitis. [2023; February 12, 2024]. Available from https://radiopaedia.org/articles/chronic-sinusitis