Adult with Hip Pain: When to Order Imaging
Case: You’re seeing a 75-year-old female with a 2-week history of right-sided hip pain. She says the pain is severe with walking and improves with rest. The location of the pain is anterior hip/groin area. She denies any recent history of fall or trauma or change in her routine activities. She has experienced this pain before, but not as severe. Historically she has low back pain due to vertebral compression fracture but she says her back pain is not bothersome today. She has osteoporosis and takes a weekly bisphosphonate medication. What is your initial differential diagnosis?
BOTTOM LINE:
Acute hip pain: <4 weeks
Sub-acute hip pain: 4-12 weeks
Chronic hip pain: >12 weeks
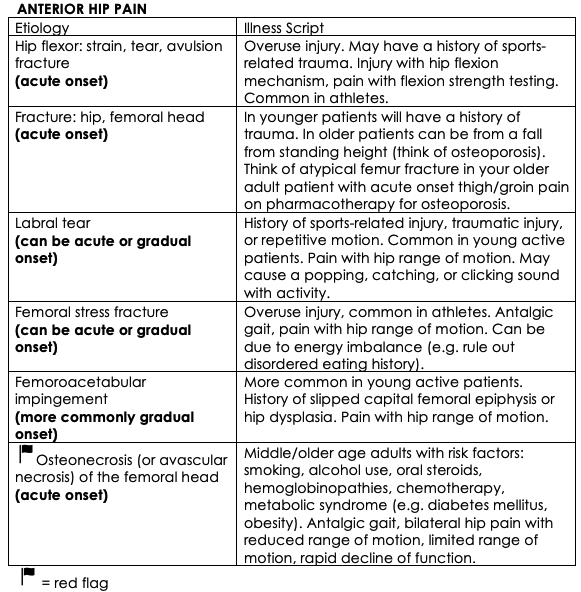
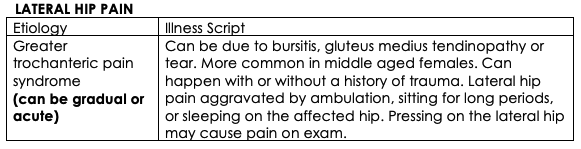
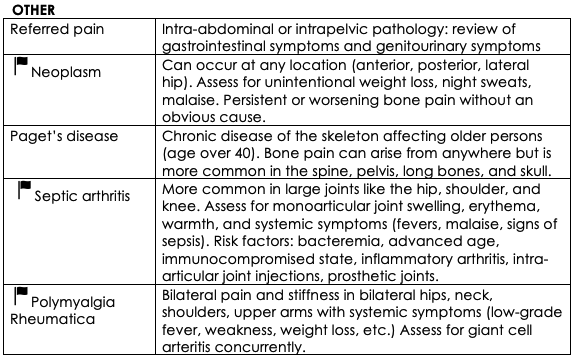
Diagnostic Approach: Hip pain has a long list of differential diagnoses. Acute hip pain lasts less than 4 weeks, subacute is between 4 and 12 weeks, and chronic lasts more than 12 weeks. Organizing your differential for hip pain using the anatomic framework can be helpful. For example, hip pain is often localized to one of three locations: anterior, posterior, or lateral (1). Knowing your illness script for each presentation can be helpful. Ask the following questions to narrow down your differential: Is this injury acute or gradual in onset? Is it bilateral or unilateral? Is my patient young or middle-aged/elderly? Does this patient have a history of trauma or recent fall from standing height? Is this a traumatic sports injury or repetitive use injury? Are there any systemic or inflammatory symptoms present?
Source: Chamberlain R. Hip Pain in Adults: Evaluation and Differential Diagnosis. American family physician. 2021;103(2):81-9.
Source: Chamberlain R. Hip Pain in Adults: Evaluation and Differential Diagnosis. American family physician. 2021;103(2):81-9.
Source: Chamberlain R. Hip Pain in Adults: Evaluation and Differential Diagnosis. American family physician. 2021;103(2):81-9.
Back to the case: she denies any radiating pain, or pain in other joints. She denies any systemic symptoms including fever, chills, malaise, weight loss, or night sweats. She has no prior hip replacement surgery. She is an older female without trauma, fall, or change in usual activity to suggest an overuse muscle injury, and she has no risk factors for osteonecrosis. She denies any gastrointestinal or genitourinary symptoms. With your history alone you have ruled out many differential diagnoses. On further questioning you learn she has been taking bisphosphonate medication for about six years.
Physical exam: Her vitals are normal. She has an antalgic gait with normal Trendelenburg sign, and there is no joint erythema, warmth, or swelling. She reports pain with right hip abduction, internal and external rotation. Remainder of the physical exam is unremarkable. You mainly want to rule out atypical femur fracture. You question what diagnostic imaging is warranted at this time.
BOTTOM LINE: Ask Yourself the Following
1) Is pain originating from the joint or is it referred pain from elsewhere?
2) Is the hip pain anterior, posterior, or lateral?
3) Is hip pain bilateral or unilateral?
4) Is this injury acute or gradual in onset?
5) Is my patient young or middle-aged/elderly?
Role for Imaging: Consideration of diagnostic imaging is dependent on your differential diagnoses and your pre-test probability. Let’s look at considerations for radiograph, ultrasound, CT, and MRI.
A good rule of thumb: many conditions will improve with conservative management (e.g. piriformis syndrome, low back pain without red flags) – if conservative management fails after 6 weeks of active therapy, re-visit your initial diagnosis, and consider diagnostic imaging.
Back to the case: a right-sided pelvic and femoral head x-ray is a reasonable, quick, and inexpensive initial test to order to rule out atypical femur fracture. Knowing this is not a perfect test, you may consider CT/MRI as second steps if initial imaging is inconclusive.
BOTTOM LINE: XRAY is a good initial test for acute hip pain but can miss many things. MRI is the most sensitive and specific test for muscle, tendon, and ligament injuries, osteonecrosis of the femoral head, septic hip arthritis, femoral stress fracture, and neoplasm.
Key Take Home Points:
Hip pain can be a nebulous concern to work up. Start with a broad differential diagnosis and perform a thorough history and physical exam.
X-ray, ultrasound, CT, and MRI all have their pros and cons. Take into consideration the diagnostic accuracy of each test and your pre-test probability before ordering.
On our clinical tools page, there is an excellent resource to refresh yourself on MSK exams, under Rheumatology called Rheumtutor.
References/readings:
Chamberlain R. Hip Pain in Adults: Evaluation and Differential Diagnosis. American family physician. 2021;103(2):81-9.
Dominguez S, Liu P, Roberts C, et al. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs- a study of ED patients. Acad Emerg Med. 2005;12:366–369.
Canadian Association of Radiologists. Canada. 2021-2022 [February, 2024]. Available from: https://car.ca/patient-care/referral-guidelines/
O'Sullivan GJ, Carty FL, Cronin CG. Imaging of bone metastasis: An update. World J Radiol. 2015 Aug 28;7(8):202-11. doi: 10.4329/wjr.v7.i8.202. PMID: 26339464; PMCID: PMC4553252.
Radiopedia. 2023. [February 2024]. Available from: https://radiopaedia.org/articles/septic-arthritis
Dawes AR, Seidenberg PH. Sonography of sports injuries of the hip. Sports Health. 2014 Nov;6(6):531-8. doi: 10.1177/1941738114552801. PMID: 25364486; PMCID: PMC4212357.
Eggenberger E, Hildebrand G, Vang S, Ly A, Ward C. Use of CT Vs. MRI for Diagnosis of Hip or Pelvic Fractures in Elderly Patients After Low Energy Trauma. Iowa Orthop J. 2019;39(1):179-183. PMID: 31413692; PMCID: PMC6604520.
Liu Y, Lu W, Ouyang K, Deng Z. The imaging evaluation of acetabular labral lesions. J Orthop Traumatol. 2021 Aug 6;22(1):34. doi: 10.1186/s10195-021-00595-7. PMID: 34357462; PMCID: PMC8346610.
Thierfelder KM, Gerhardt JS, Gemescu IN, Notohamiprodjo S, Rehnitz C, Weber MA. Imaging of hip and thigh muscle injury: a pictorial review. Insights Imaging. 2019 Feb 15;10(1):20. doi: 10.1186/s13244-019-0702-1. PMID: 30771029; PMCID: PMC6377690.
Albers CE, Wambeek N, Hanke MS, Schmaranzer F, Prosser GH, Yates PJ. Imaging of femoroacetabular impingement-current concepts. J Hip Preserv Surg. 2016 Nov 10;3(4):245-261. doi: 10.1093/jhps/hnw035. PMID: 29632685; PMCID: PMC5883171.