Understanding Lab Reference Ranges: A Primer
We order lab tests for various reasons – to confirm or refute a diagnosis, to screen for disease, to determine the severity of disease, for treatment response, and medication monitoring. Interpreting results (especially unexpected or incidental findings) can be challenging. Understanding test accuracy principles (sensitivity and specificity, negative and positive predictive value, likelihood ratios, pre-test probability) are integral for appropriate use of diagnostic tests.
Specific to lab testing, it’s important to understand how lab reference ranges (or reference intervals) are established. Understanding how reference ranges get established, and their limitations, can help with how we interpret results. Let’s use a case example.
Case: A CBC was ordered for a 40-year-old male presenting with fatigue. Hemoglobin results are reviewed.
Hgb: 175g/l (17.5g/dl)
What is a reference range? It is the interval between two reference limits – the highest and lowest value in a number set.
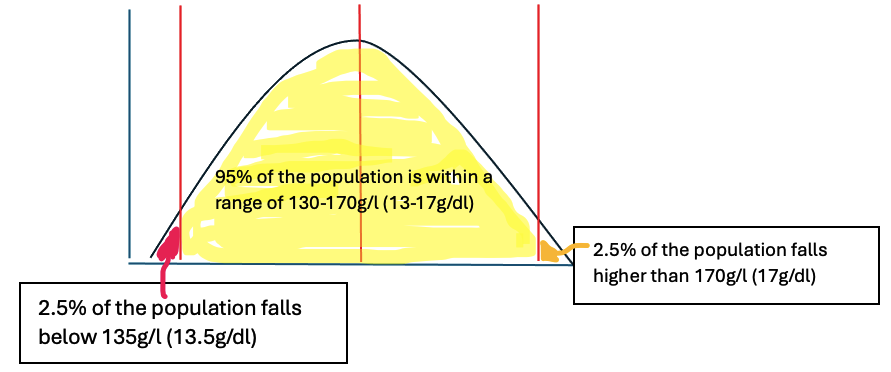
How are lab reference ranges established? Many lab tests are expressed as a number that falls within a reference range. Reference ranges are established by testing large groups of healthy people to determine a “normal” range for that group (1). A sufficient number of healthy individuals distributed over a range of age and sex is required to establish a reference range (2). The central 95% of results is used (i.e., 2.5% to 97.5%) with an appropriate statistical technique, either parametric or nonparametric, to determine the reference range (2).
In other words, a group of “healthy” individuals’ results are taken to create a mean under a standard distribution curve, with 2.5% of people falling below the lowest number, and 2.5% of people falling above the highest number.
What are the limitations of reference ranges? Clinical biochemists provide references ranges that are as robust as possible, but there are difficulties in establishing reliable reference ranges (2). This means the numbers we use to interpret lab results are not perfect. Reference ranges are periodically adjusted based on new evidence, and labs subsequently adjust their reference ranges.
When constructing reference ranges, it’s important to define who is “healthy” and to consider the importance of subclinical disease states (2). It is difficult to establish what “good health” means, as it is a relative concept, and even more difficult to select “healthy” individuals. For example, an individual may subjectively feel they are in good health, but in fact have subclinical disease (e.g. untreated hypertension).
If any result falls outside the range, we may consider this as clinically important. We may not consider that a borderline result outside the analytically valid reference range sometimes requires verification or surveillance versus immediate prescribing or investigating. On the contrary, a perfectly healthy person’s lab result can fall outside the established reference range. Studies used to establish the reference range are not perfect, and there are select people in a population that simply fall outside of the standard distribution. In other words, an abnormal results does not always equal disease. Further, “normal” reference ranges differ from lab to lab.
Limitations of lab reference ranges:
Derived from imperfect studies of healthy populations
Establishing what “healthy” means is relative
Healthy individuals may have subclinical disease states
Falling outside the reference range does not mean you have the disease
Why do lab reference ranges vary from lab to lab? Labs use different types of equipment and tests, and sometimes they set their own reference ranges. We use the reference range reported from the lab used for the test in everyday practice. For example, some labs will use a reference range of 135-170g/l (13.5-17g/dl) for hemoglobin (3), others might use a slightly difference reference range 140-170g/l (14-17 g/dl) (4). We should always consider the possibility of a lab error if results return and do not correlate clinically.
Back to the case: a hemoglobin of 175g/l (17.5g/dl) is high and considered outside the reference range. You go down a basic differential for increased hemoglobin values (dehydration e.g. diuretics, vomiting, diarrhea, primary and secondary polycythemia vera, hypoxia from pulmonary disease, sleep apnea, cardiovascular disease e.g. heart failure, high-altitude, endocrine disorders e.g. pheochromocytoma, exogenous erythropoietin) (5). The remainder of the CBC indices are within reference range. Your patient has no past medical history and takes no medications. He has no recent history of illness (e.g. shock, diarrhea, dehydration) or blood transfusions. He has no symptoms suggestive of sleep apnea, cardiovascular disease, respiratory disease, or pheochromocytoma. He denies use of exogenous EPO.
In this case, repeating the CBC is reasonable before investigating further (5). You decide to repeat the CBC in a month. It returns as 170g/l (17g/dl) – now within the reference range. You have ruled out an abnormal hemoglobin as the cause (i.e. anemia). You continue the work up for fatigue.
As you can see from this case, we often order a CBC as part of a routine work up for a patient presenting with fatigue. The rationale is to rule out anemia. When we receive an unexpected result – in this case, a high hemoglobin – this can throw us a curve ball.
If an unexpected or incidental result returns, ask yourself the following:
Does the result make sense clinically? (i.e. based on history, physical exam findings, correlation with other test results)
Could it be a lab error?
Could this person simply fall outside the predetermined reference range (i.e. they are healthy)?
This was an introductory post, which will set the stage for how we can interpret various lab tests using the imperfect reference ranges we have.
References
Alberta: HealthLinkBC. Understanding Lab Test Results. [Internet]. [cited 2024 April 15]. Available from https://www.healthlinkbc.ca/health-topics/understanding-lab-test-results
CMAJ: Topliss DJ. What happens when laboratory reference ranges change? Canadian Medical Association Journal. 2020 May;04 192(18):E481-E482. doi: https://doi.org/10.1503/cmaj.200511 (access here: https://www.cmaj.ca/content/192/18/E481.short)
BC: BC Cancer. Lab Test Interpretation Table. [Internet]. [cited 2024 April 15]. Available from http://www.bccancer.bc.ca/pharmacy-site/Documents/Clinical_Pharmacy_Guide/cpg3e-lab-test-table.pdf
Merck Manual Professional Version. Blood Tests: Normal Values. [Internet]. [cited 2024 April 15]. Available from https://www.merckmanuals.com/en-ca/professional/resources/normal-laboratory-values/blood-tests-normal-values
Tefferi A. Diagnostic approach to the patient with erythrocytosis/polycythemia. In: UpToDate, Eidt Larson RA, Rosmarin AG (Ed), Wolters Kluwer. (Accessed April 15, 2024).