Should I Order Imaging for Low Back Pain?
Case: a 50-year-old male presents with a 1-week history of low back pain.
How can we conceptualize low back pain? It’s a symptom that results from several pathologies (1). There are multiple contributing factors (e.g. genetic, psychological, social, other co-morbidities) and pain-processing mechanisms) (1). In most patients, no specific nociceptive or clear pathological cause is found (1).
Differential Diagnoses: before assessing your patient, you have a list of potential differential diagnoses for acute low back pain (defined as <6 weeks duration) (2). I like to organize my differential for low back pain using the mechanisms approach.
What Mechanisms Cause Low Back Pain?
Taking a Good History for Low Back Pain
Consider these key questions to elicit an accurate history (sometimes you have the ask the same question a few different ways to get the right information!)
When did the pain start?
What is the location of the pain?
Does the pain radiate anywhere else?
Is the pain constant or intermittent?
What movements make the pain worse? (flexion, extension, walking/standing, all movements)
What movements make the pain better? (flexion, extension, walking/standing)
Have you had this type of back pain before?
Have you had a fall recently, or an accident (e.g. car accident)?
Do you feel weakness in your legs?
Have you had any unexpected accidents with your bowel or bladder function since this episode of low back pain started?
Are you experiencing stiffness in your back for longer than 30 minutes upon waking in the morning? Does movement improve your back pain?
Do you have any fevers or chills since the back pain started?
Do you use IV drugs?
Do you have a history of cancer?
Have you lost weight without meaning to?
Do you have severe fatigue since the back pain started?
Do you have severe back pain at nighttime (that is worse than daytime pain)?
*If a person has had low back pain for longer than 6 weeks, assess for “yellow flags” which can help tease out psychosocial risk factors for developing chronic back pain (1,3).
PEARL #1: Rule out the red flags, and narrow in on whether your patient fits one of the 4 common patterns of mechanical back pain.
Back to the Case: he was shoveling snow a week ago when he felt immediate pain over the right lumbar region. The pain is constant and intermittently radiates down the right leg. The back pain is more bothersome than the leg pain. It hurts most to bend forward, and he gets some relief with back extension. He has felt intermittent tingling and numbness radiating down the right leg into the great toe. He denies any weakness or difficulty walking or standing. There are no red flags on review of systems.
Physical Exam for Low Back Pain
The CORE back tool provides an excellent review of the physical exam (3). As a quick overview, always assess the following: gait, heel walking, toe walking, inspection, palpation, range of motion, strength, reflex testing (patellar, achilles, Babinski), and special tests (straight leg raise).
Back to the Case: antalgic gait is noted, with limited forward flexion (secondary to pain), pain over the lumbar spine and right paraspinal muscles on palpation. Otherwise, the physical exam is unremarkable. He asks you whether you can order an x-ray for him to “make sure everything is OK.”
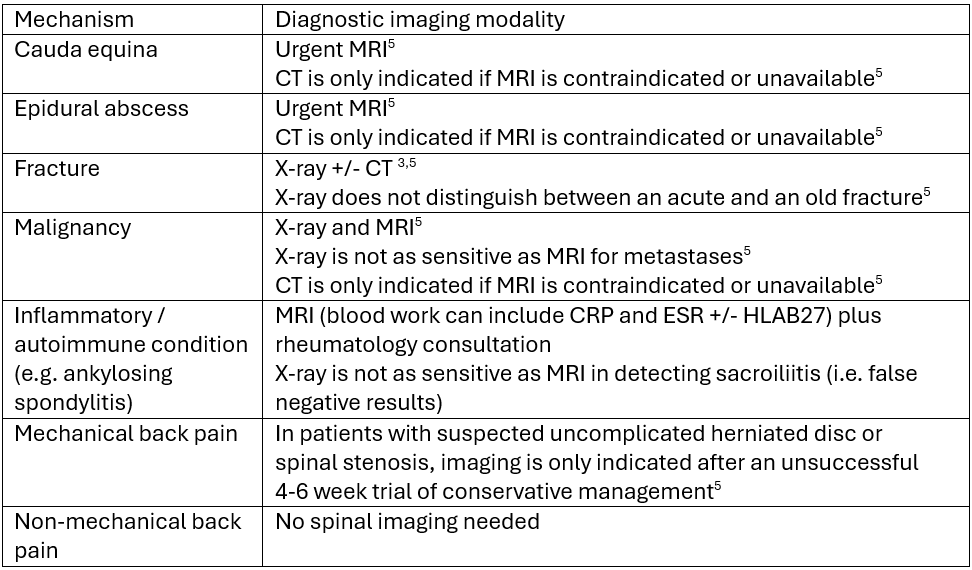
Diagnostic Imaging for Low Back Pain
Low back pain is a self-limited condition that does not require imaging for uncomplicated cases (i.e. no red flag signs or symptoms resolve at 6 weeks of conservative management) (2).
Imaging should only be considered if 1) patients who have had up to 6 weeks of medical management and physiotherapy have had no improvement in symptoms (as imaging may change management); and 2) patients have red flags for serious pathology (4).
Let’s break it down:
PEARL # 2: Lumbar spine imaging is only indicated in the presence of red flags OR if pain is persisting despite active conservative management at 4-6 weeks (e.g. compliance with physiotherapy).
When is a Surgical Referral Appropriate?
Failure to respond to conservative management of at least 12 weeks
Unbearable constant leg dominant pain
Worsening nerve irritation tests (e.g. straight leg raise)
Worsening motor, sensory, or reflex deficits
Recurrent disabling sciatica
Disabling neurogenic claudication
(3)
Back to the case: you diagnose your patient with mechanical low back pain, likely pattern 1, disc pain (aggravated by flexion, relieved with extension). You explain the diagnosis, prognosis, and treatment recommendations. You provide him with a rationale that diagnostic imaging would not change management (6). You review red flags and when to present to the emergency department and instruct him to follow up in 6 weeks if the pain has not resolved.
Interpreting Findings on Radiology Reports: Lumbar Spine MRI
If we order a lumbar spine MRI, we need to know how to interpret the findings and determine whether it correlates clinically or not. First, let’s review lumbar spine anatomy to make sense of radiology reports. Most adults have 5 lumbar vertebrae (L1-L5), and 5 sacral spinal nerves (S1-S5). Each vertebral body stacks on top of each other to form the spinal canal which contain a pair of nerve roots (one on the left and one on the right) (7). Each nerve root passes through a small bony tunnel called the neural foramen as they exit the spinal cord (7).The lumbar nerve roots innervate the pelvis and lower limbs. An intervertebral disc sits in between each vertebrae. The disks are made up of the nucleus pulposus, which provides cushioning to the spinal column and the annulus fibrosus, which is a fibrocartilaginous ring that keeps the nucleus pulposus intact when forces are applied to the spinal column (7). Facet joints link each level of the spinal column. If you need a visual recap, this video is helpful (7).
Pearls for understanding findings on MRI:
Annular fissure: any separation between annulus fibres or avulsion of annulus fibres, often occurring in the setting of asymptomatic disc degeneration. This is a degenerative change that may not correlate clinically with back pain (8).
Disc herniation: any disc material extending beyond the vertebral body is considered herniated. Common terms used are disc bulge, protrusion, extrusion, or sequestration on radiology reports. The relation of the herniated disc to the nerve root is examined, in attempts to correlate the back pain clinically (8).
Vertebral canal stenosis (also reported as spinal stenosis or neural foraminal stenosis): the canal which contains the pair of nerve roots becomes too narrow and creates pressure on the spinal cord and nerve roots. Clinically, this would correlate with progression of decreasing mobility and neurogenic claudication. In acute circumstances, the initial presentation may occur as cauda equina where urgent surgical decompression is required (8).
Spondylolisthesis: malalignment of the lumbar spine in the form of a vertebra slipping out of its normal position relative to the inferior vertebra – this can cause severe central canal and neural foraminal stenosis and associated nerve impingement (8).
Facet joint osteoarthritis: there may not be any correlation between imaging findings and low back pain (1).
Ankylosing spondylitis diagnostic hints: common features include bone marrow edema, squaring of the vertebral bodies, syndesmophyte formation, ankylosis and erosions (8).
PEARL #3: Make sense of the radiology report – do the findings correlate clinically?
References Feger J, Sciacca F, Knipe H, et al. Low back pain. Reference article, Radiopaedia.org (Accessed on 30 Sep 2024) https://doi.org/10.53347/rID-92309Lancaster B, Goldman J, Kobayashi Y, Gottschalk AW. When Is Imaging Appropriate for a Patient With Low Back Pain? Ochsner J. 2020 Fall;20(3):248-249. doi: 10.31486/toj.20.0077. PMID: 33071654; PMCID: PMC7529135.Center for Effective Practice (2016). Clinically Organized Relevant Exam (CORE) Back Tool. Center for Effective Practice. https://cep.health/tool/download/19/ACR: Patel ND, Broderick DF, Burns J, et al. ACR appropriateness criteria low back pain. J AmColl Radiol. 2016. Sep;13(9):1069-1078. doi: 10.1016/j.jacr.2016.06.008.Canadian Association of Radiologists. Canada. 2021-2022. Available from https://car.ca/patient-care/referral-guidelines/Choosing Wisely (n.d.). Imaging tests for low back pain. Choosing Wisely. https://choosingwiselycanada.org/pamphlet/imaging-tests-for-lower-back-pain/https://www.youtube.com/watch?v=0qR-Yfw9fOI
Yong, X Z. & Sutherland, T. (2012). Making sense of MRI of the lumbar spine. Australian Family Physician. https://www.racgp.org.au/afp/2012/november/making-sense-of-mri-of-the-lumbar-spine