When Should you Order Imaging for a Patient with Neck Pain?
Neck pain is a common patient presentation – although most causes are benign, there are some important diagnoses to consider.
Case: You’re seeing a 40-year-old female with a 4-week history of neck pain. She reports intermittent tingling and numbness that radiates into her right arm to her fingertips. She works on a factory line that requires repetitive lifting.
Diagnostic Approach to Neck Pain
History: 1) break it down into acute (<6 weeks), subacute (<3 months) or chronic (>3 months); 2) Is it mechanical (e.g. myofascial pain, trapezius strain), neuropathic (e.g. herniated disk, spinal stenosis), or from a secondary cause (e.g. c-spine compression fracture)? 3) How is it affecting the persons activities of daily living?
Exam: Inspection – Palpation – Range of motion – Special tests. Remember to assess both the head, neck, and upper extremities. Perform a full neurological exam if onset is acute, if traumatic, moderate/persistent pain, referred shoulder/arm pain, or if red flags are present.
Back to the Case: You note tenderness on palpation of paraspinal and trapezius muscles, and a positive spurling test with her neck rotated to the right. Neurological exam is normal. You are fairly certain she has acute right sided cervical radiculopathy, and neck muscle strain. You question whether you need to order any imaging.
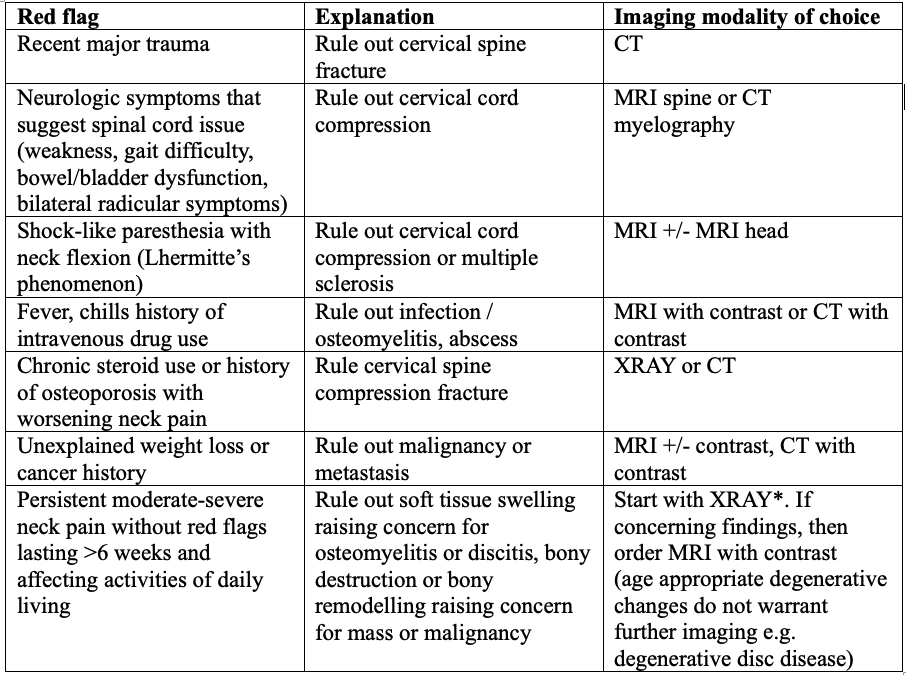
Red flags of Neck Pain and when to Consider Ordering Imaging (1)
*TIP: for patients with spinal hardware, x-ray is the first imaging modality of choice.
Back to the Case: your patient has sub-acute neck pain without red flags, so you forego diagnostic imaging for the time being and recommend a trial of conservative management.
When should we NOT order imaging?
1) Unilateral cervical radiculopathy without red flags <6 weeks duration - trial conservative management first.
2) Musculoskeletal etiology suspected - trial conservative management first.
3) Non-spinal cause of neck pain suspected - go down a different diagnostic pathway if it does not sound like a spinal source of pain (e.g. anterior neck pain could be angina, associated jaw pain or visual changes could be giant cell arteritis).
A note on the Canadian C-Spine Rule: if you work in an acute care setting and encounter an alert (GCS 15) and stable trauma patient where cervical spine injury is a concern, you can use the Canadian C-Spine Rule to determine the need for radiography.
Key take Home Points
1) If a patient has neck pain with red-flags, particularly if the presentation is acute, they should be urgently assessed in an acute care facility as the consequence of misdiagnosis is high.
2) If you are ordering imaging tests, consider spine imaging if you think the pain is originating from the central nervous system and there are either a) red flags present, or b) the patient reports moderate to severe pain lasting >6 weeks that is affecting their quality of life.
Resources/References
1. Cohen SPMD. Epidemiology, Diagnosis, and Treatment of Neck Pain. Mayo Clinic proceedings. 2015;90(2):284-99. (VIEW HERE).
2. Canadian Association of Radiologists. Canada. 2021-2022 [July, 2023]. Available from: https://car.ca/patient-care/referral-guidelines/
3. What is the spurling test? Find out HERE.